Pediatric Orthopedics
Apophysitis
Apophysitis refers to irritation and inflammation of the apophysis, a secondary ossification center which acts as an insertion site for a tendon. It is a common overuse injury in young athletes. In a growing athlete, the apophysis is susceptible to injury because of repetitive stress or an acute avulsion injury. An avulsion fracture usually occurs with sudden muscle contractions where a small piece of bone is torn away from its origin.
During rapid growth period, the ability of the muscle tendon unit to stretch decreases compared to bone growth resulting in increased tension at the attachment site. In the young athlete, because of training and participation in multiple sports a traction force at the apophysis is exaggerated. Certain conditions such as pronation of the foot or genu valgum may aggravate abnormal forces at the apophysis and result is apophysitis.
Apophysitis can occur at the hip and pelvis, knee, and foot. Pelvic or hip apophysitis is often seen in individuals aged between 14 and 18 years. Risk of pelvis/hip apophysitis is more in individuals having excessively tight hip and thigh muscles. Pelvic bone has many apophyses and any of these may affected. However, apophysitis of anterior superior iliac spine, anterior inferior iliac spine and iliac crest apophyses is more common.
Apophysitis of the knee is known as Osgood-Schlatter disease. Osgood-Schlatter disease is characterized by swelling, pain and tenderness just below the knee, over the shin bone (tibia). It is commonly seen in young adolescent boys who participate in certain sports, such as soccer, gymnastics, basketball, and distance running.
Apophysitis of the foot is known as Severs disease. Severs disease, also called as calcaneal apophysitis is a condition that affects growing adolescents causing inflammation of the growth plate of calcaneous bone, a bone at the back of the heel. The condition can affect both heels and most commonly occurs in boys between the ages 8 and 13.
Children with apophysitis may complain of pain that may occur gradually without a particular history of injury. The symptom tends to worsen after a single traumatic event. These symptoms decrease once growth at the apophysis is complete.
Your doctor will diagnose apophysitis based on history and physical examination. X-rays may be needed to rule out other conditions such as infection or tumor. The goal of the treatment is to relieve the pain and to treat the underlying factors. Avoid activities that worsen the pain and protect the apophysis from further injury. Participating in sports is not allowed as long as limping is present during walking or during activities. An open growth plate is more susceptible to injury and hence lack of protection of the apophysis can result in an avulsion fracture. A rehabilitation program that includes home exercise program and physical therapy may be recommended to improve strength and flexibility.
Muscle Strains
Muscle strains are more common injuries in sports. Muscle strain refers to an injury of a muscle or its attaching tendons. A tendon is a tough, fibrous cord of tissue that connects muscles to bone. There are two types of muscle strains, acute strain and chronic strain. Acute strains are caused by excessive stretching or tearing of a ligament. Chronic strains are caused by repetitive movements of muscles and tendons over long periods of time and are more common in tennis players and golfers.
Sports activities such as football, basketball, hockey, gymnastics, boxing, wrestling, tennis, rowing, golf-sports, racquet, throwing, and contact sports place participants at greater risk for strain. The symptoms of a strain are typically pain, swelling, muscle spasm, muscle weakness, inflammation, and cramping.
Back strain occurs when the muscles supporting the spine (back bone) are twisted, pulled or torn. Athletes involving in excessive jumping as in basketball or volley ball are more susceptible to back strain.
Hamstring muscle strain is a tear in one or more of the muscles at the back of the thigh. It is caused by imbalance between the hamstrings and the muscles in the front of the thigh. Sports that commonly cause a hamstring injury are sprinting sports such as track and field, soccer, and basketball that involve sudden accelerations.
Most sprains and strains will repair themselves with adequate rest, ice application, compression, and elevation. In case of severe injury, a brace or a splint may be used to immobilize the area and to prevent further injury. Surgery is occasionally required to repair the ruptured muscle or torn ligament.
Prevention
The following tips can help reduce the risk of developing muscle strains:
- Sufficient stretching of lower and upper back muscles or warm-up exercises before playing sports is necessary
- Follow an exercise program to strengthen the muscles
- Eat a healthy well-balanced diet that nourishes muscles
- Always wear a proper fitting athletic shoe with good support
- Use proper equipment suitable for the sport you play
In Toeing
Description
- In-Toeing is very common in children and may occur at various times during childhood development
- In toeing may also be referred to as pigeon feet
- The condition may occur because of an inward twisting along various areas of the leg including the hip, thigh, shin, and foot. Where this occurs along the leg is highly correlated with age, posture, sex, and particularly sitting position
- Most of these conditions are benign, do not require surgical treatment, and resolve as the child ages, typically by 8 to 10 years of age
Types of In Toeing

- Metatarsus Adductus - also known as inward twisting of the foot, is a condition where the bony distal parts of the foot are turned inward. The condition is usually seen in the first year of life due to limited space of the uterus during growth and development of the fetus. Standing examination reveals normal hip, knee, and ankle alignment.
- Internal Tibial Torsion - a condition in which the tibia (shin bone) is turned inward as a result of sleeping or sitting positions. The condition is usually seen by age two and is most apparent when the individual begins to walk. Standing examination reveals normal hip and knee alignment, but inward rotation of the foot and ankle
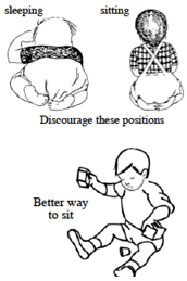
- Femoral Anteversion – a condition in which the femur (thigh bone) is turned inward. Femoral anteversion is twice as common in girls, usually occurs between the ages of 3 to 6, and has a high association with sitting position. Many children affected by this condition sit in the "W" position. Standing examination reveals inward rotation of the ankles, feet, and particularly the knees.


Treatment
- Regardless of the location of inward rotation, most children outgrow the condition by the time of adolescence. In the past, complex shoes, braces, or castings were used to correct the deformity, but current research has steered away from this.
- Correction in sitting posture is very beneficial in resolving these conditions
- In very rare instances is surgical intervention indicated. Surgery usually entails fracturing a bone at the involved segment of the leg, rotating to make the leg straight, and applying a cast to allow the bone to heal in the correct position. This is usually not needed as most children outgrow their in toeing
- Metatarsus adductus treatment – usually only involves observation and rarely is a correcting orthopedic shoe, cast or surgery indicated
- Tibial torsion treatment – discouraging the child from sitting or sleeping on her or her feet will promote resolution of this condition. In severe cases, a night brace (such as the Denis Browne bar or Friedman splint) may be prescribed for the child to wear to prevent the child's feet from curling underneath them
- Femoral Anteversion treatment – the best treatment is to instruct children to sit in the "Indian" or "legs criss-cross applesauce" position as opposed to the "W" position

Flatfoot in Children
Description

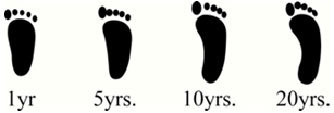
- A flatfoot is a foot with a low or absent arch along its inner border. In an otherwise normal child, this condition is known as flexible flatfoot
- Varying degrees of flexible flatfoot are to be expected at some point in a child's life, particularly in the first few years of life
- Despite having the potential to cause the parent much distress, this condition is very common in young individuals and most outgrow the condition with age
Diagnosis
- A general exam of the child is used to make a diagnosis of flexible flatfoot. The exam includes an evaluation of
- Gait and ability to walk on the heals and tips of toes
- The degree of laxity in the child's ligaments
- Neurological status
- Limb alignment and foot anatomy
- During the exam, the child will be asked to stand on his or her tiptoes. During this stance, the arch will be recreated in individuals with flexible flatfoot
- Radiographic imaging may be used to assess flatfoot severity, but is not typically required in mild cases
Treatment
- Current medical literature shows no benefit of corrective shoes or arch supports in the treatment of flexible flatfoot.
- In the setting of pain, an ill-fitting shoe is like treating a headache with rock music. On the other hand, a proper fitting athletic shoe is like classical music to help soothe the discomfort. Thus, properly fitted athletic shoes are very important in preventing injury and reducing pain
- In some instances, an over-the-counter orthotic may be suggested to provide comfort. Blue Insole Superfeet are fairly inexpensive and widely available (at Sports Chalet, Chick's, REI, and Nordstrom's)
- Surgery is only recommended in rare instances. Most children that require surgical intervention have severe flexible flatfoot and are not considered for surgery until 8 to 9 years of age

Regardless of the treatment, the child should be regularly checked by his or her orthopedist to ensure proper bony growth and development
Click on the topics below to find out more from the Orthopedic connection website of American Academy of Orthopaedic Surgeons.
Deformity
Limb Deformities
Limb deformities are conditions that affect the bones, muscles and tendons of the upper and lower limbs. Most of the conditions are generally asymptomatic, except for a cosmetic concern. Some are harmless and self-correcting in nature or may sometimes require simple treatment. Some deformities, however, are complex and are corrected by surgery. Limb deformities can be congenital- present at birth or may occur at a later stage as a result of fracture, infection, arthritis or tumor. Congenital deformities of the lower limbs are the developmental disorders that cause alteration in the shape and appearance of the legs. There are several factors such as genetic factors which influence the fetal growth in the womb and teratogenic drugs and chemicals that can cause congenital deformities.
Some of the deformities of lower limb and corrective procedures include:
Calcaneovalgus foot: This postural deformity is located at the ankle joint and the foot appears to be bent upwards. The foot appears flat and the heel bone turns outwards. The treatment depends upon the severity of the condition. In mild cases, gentle stretching exercises and massage to the foot performed by the parent can help. Splinting can be done in moderate cases and if there is no improvement with stretching exercises after 1-2 months. In cases of severe deformity, serial casting is needed for up to 3 months. Then splints are given to be worn only in the night for 2-10 weeks as a part of maintenance therapy.
Congenital Vertical Talus (CVT): CVT is also known as Rocker-Bottom foot, is a rare condition and is often mistaken for calcaneovalgus, but it is a rigid deformity and not as flexible as calcaneovalgus foot. The initial treatment starts with serial manipulations and application of casts. Cast treatment can only improve the deformity. Definitive correction can be achieved by a soft-tissue release operation. The type of surgical procedure performed depends on the age of the patient, severity of the deformity and surgeon's preference. In children up to the age of three, open reduction of the talonavicular joint is traditionally done. Children between the ages 4 and 8 are usually treated with open reduction combined with extraarticular arthrodesis (surgical fusion of joint). Patients above 8 years may require a triple arthrodesis.
Congenital clubfoot (Talipes equinovarus): Congenital clubfoot is the most common and obvious of all the foot deformities. The feet may become twisted inwards in such a way that top of the foot comes in place where the bottom should be. The initial treatment for clubfoot is the use of non-surgical methods such as serial manipulation and casting using the Ponseti method, taping, physical therapy and splinting, and continuous passive motion with a machine. Surgical correction is required in severe cases that do not respond to stretching and may include release of soft tissue and joint contractures, tendon lengthening, and fixation of temporary pins in the foot.
Flat foot (Pes planus): Flat feet, also known as pes planus is a deformity of the feet, in which the arch running lengthwise along the sole of the feet has collapsed or has not formed at all. Non-surgical treatment options include activity modification, orthotic devices, physical therapy, medications and shoe modification. Surgical procedures may be performed and can include tendon transfers, tendon lengthening, bone realignment, joint fusion, or implant insertion.
Metatarsus adductus: In this condition, the forefoot is bent or turned inwards towards the midfoot. The lateral side (outer border) of the foot is curved making the foot appear like a kidney bean. If your child's foot is flexible enough to be straightened, no further treatment is required other than periodic follow-ups. In cases where the problem does not improve, stretching exercises of the foot will be taught and your child may have to wear a splint or special kind of shoes called "reverse-last shoes". Casts if needed will be placed before the child is 8 months old, as better results can be achieved during this period. Surgery may be required in rare cases.
Tarsal coalition: Tarsal coalition is a developmental deformity that occurs because of fusion between two bones (tarsal bones) at back of the foot. The non-surgical methods include use of orthotic devices, physical therapy, injection of anesthetic agent and nonsteroidal anti-inflammatory medications (NSAID's). Surgery involves resection of the bony fusion to establish normal range of motion.
Leg length discrepancy: Leg length discrepancy is a condition in which one leg is shorter than the other leading to problems in posture and walking pattern. There may be associated pain in the back, hip knee or ankle. It can be corrected by a reconstructive procedure called limb lengthening during which the deformed bone is lengthened by replacing the lost bone.
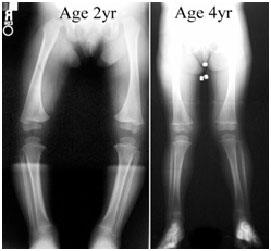
Congenital genu varus (bowed legs): It is a normal variation in the appearance of the legs seen in children below 2 years and gradually improves by the age of 3 to 4 years. Night splints may be given or osteotomy can be performed in severe cases.
Congenital Hip Problems: Congenital hip problems that can affect children are of two types, femoral anteversion and developmental dysplasia of the hip (DDH). Femoral anteversion is the condition in which the femur (thigh bone) becomes twisted inwards causing the child's knees and feet to turn inwards (“pigeon-toed” appearance). Usually, no treatment is required as the defect is self-correcting. Surgical treatment may be considered if the condition is severe and the child is above the age of 8. The surgery called, femoral derotation osteotomy is done which involves cutting the femur bone and rotating it to bring it to correct position. Developmental dysplasia of the hip (DDH) is a condition in which the femur (thigh bone) partially or completely slips out of the hip socket causing dislocation at the hip joint. Pavlik harness is used in newborns and infants below 6 months of age in order to hold the hip joint in place during growth of the child. Surgical treatment for this condition includes closed reduction with hip spica casting and open reduction.
Bowlegs & Knock-Knees
Definition
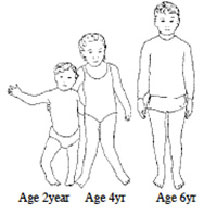
- The development of bowlegs and knock-knees is a normal part of childhood development and is usually not a concern
- Genu Valgum, also known as knock-knees, is when the legs are held straight, the angle of the knees touch. Mild genu valgum is very common in children from age 2-5.
- Genu Varum, also known as bowlegs, is when the legs are held straight, the knees are far apart with each leg giving the appearance of an archer's bow. The condition is very common between birth and the age of 3.
- Though usually symmetric, sometimes only one leg is affected
- Despite possibly causing stress in the parent, these conditions are both common and self-limited - meaning that the child's legs will develop a more straight appearance from ages 6 to 10. Some mild variations persist in the adult and may differ between sexes.
- If the conditions persists in to adulthood, the individual may be more prone to injury, chronic knee pain, and osteoarthritis
- In rare instances are these conditions associated with underlying disease or permanent deformities. Further inspection is indicated when a child develops difficulty walking, the condition persists as they continue to age, or presents with other alarming symptoms
Examination
- The diagnosis of bowlegs or knock-knees is made by visual examination while standing and observing the child walk
- Rarely, radiographs are ordered to rule out underlying bony abnormalities
- The presence of alarming symptoms or atypical presentations may indicate a metabolic work up to rule out other disease processes
Treatment
- The most common treatment of both conditions is to observe the child over time.
- No amount of orthotic treatment or strength training will correct bowlegs or knock-knees, in either the child or the adult. Thus, special shoes or braces are not advised
- Very severe cases that persist past the age of 8 or 10 can be surgically corrected by temporarily stopping one side of the growth plate with a removable plate. When proper alignment is achieved, the plate is removed
Click on the topics below to find out more from the Orthopedic connection website of American Academy of Orthopaedic Surgeons.





